When researching cosmetic procedures, it can be confusing when terms like plastic surgeon and cosmetic surgeon are used interchangeably. Although these medical specialties do share some common ground, their philosophies, research and training are distinct from one another.
Knowing the difference between a cosmetic surgeon and plastic surgeon can help you choose the right doctor for your procedure.
Qualifications
When it comes to finding a surgeon who is qualified and experienced in the procedures you want. It’s important to understand the differences between cosmetic surgery and plastic surgery. The terms are often used interchangeably, but the distinctions are important for patients to know.
According to a 2017 study, most individuals were confused by the use of varying terminology. For instance, 87 percent of the respondents incorrectly thought that special credentials and additional training are required for a doctor to call themselves an aesthetic, cosmetic, or plastic surgeon. This is not the case. While a board certified plastic surgeon has completed a residency and two-year plastic surgery fellowship, these programs typically do not include cosmetic surgery training.
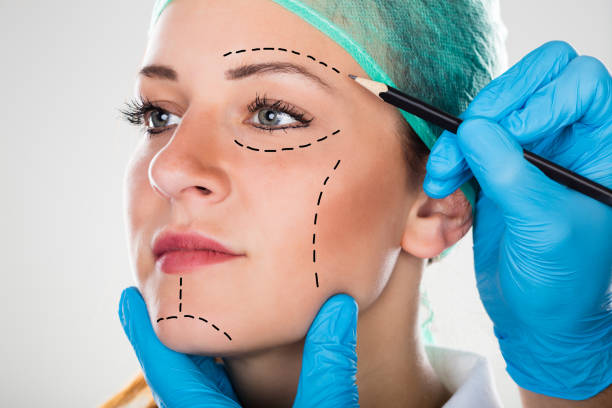
Cosmetic surgery is the process of enhancing a person’s appearance using surgical techniques that focus on improving structure and function. It is considered an elective procedure, meaning that it is not covered by insurance providers. This is in contrast to reconstructive plastic surgery, which is typically deemed medically necessary after trauma or an illness.
During your consultation, it’s important to compare physicians’ backgrounds, education, and board certifications to find the right one for your needs. You can also ask for referrals from friends or family members who have undergone similar procedures. In addition, you should ask about a physician’s post-residency training and practice history to assess their level of expertise in the specific procedures you’re considering.
Procedures
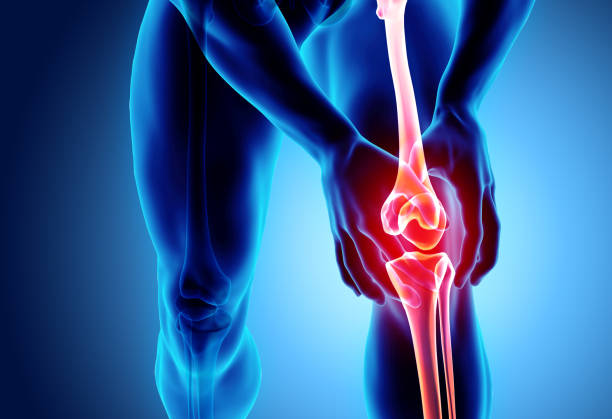
The main difference between cosmetic surgeon and plastic surgeon is that the latter offers elective procedures for aesthetic purposes. Plastic surgery on the other hand includes reconstructive procedures like cleft lip and palate repair, breast reconstruction after mastectomy, skin flaps for burns, hand surgery, and facial surgeries to help patients with conditions such as scoliosis.
While both types of surgeons have the skill to perform the procedures you want, it is important that you do your research before choosing a physician. You should look at the doctor’s credentials and training, as well as patient reviews and before and after photos to find a surgeon you trust. If you’re considering a cosmetic procedure, you should choose a board certified plastic surgeon who can offer you a wide range of options.
It is easy to see why the terms cosmetic surgeon and plastic surgeon can be confusing, as they are often used interchangeably. But, it’s important to understand that there is a significant difference between the two titles, as this can have an impact on your results and recovery time. Plastic surgeons have extensive surgical training and experience, which gives them the expertise to provide a variety of reconstructive and cosmetic procedures. They also have the knowledge and understanding to meet a patient’s individual needs. This is something that many cosmetic surgeons lack.

Recovery
The difference between cosmetic surgery and plastic surgery may seem minor, but there are important distinctions that can be made when researching prospective surgeons. While both surgeons specialize in improving the body, their training and research focus are very different. This is a crucial fact to understand, as it could affect your recovery time and results.
Plastic surgery is a medical specialty that encompasses reconstructive work as well as aesthetic improvements to the face and body. It focuses on restoring damaged or abnormal body parts, like injuries caused by trauma/accidents or birth defects. It is often considered a medically necessary procedure and may be covered by health insurance.
Cosmetic surgery, on the other hand, is an elective procedure that enhances a patient’s appearance. It is often requested by patients to correct imperfections or reshape certain areas of the body for a more attractive look. Cosmetic procedures include breast lifts, tummy tucks and facial rejuvenation.
Cosmetic surgeries are generally performed on an outpatient basis and require a shorter recovery period than many other types of surgical procedures. It is important to follow the aftercare guidelines provided by your surgeon to ensure a smooth and healthy recovery. For example, it is important to avoid alcohol and heavy exercise while recovering from cosmetic surgery. These activities can delay the healing process and increase the risk of complications.
Costs
The costs associated with plastic surgery vary widely. Some surgeons may separately bill components, such as facility fees and anesthesia fees, which can quickly add up. Dean White plastic surgeon is committed to providing transparent pricing and will only charge for what is needed to perform your procedure safely and effectively.
We encourage you to seek out quotes for your cosmetic procedure from multiple surgeons. However, you should be wary of prices that appear too low as this could indicate a lower standard of care. In many cases, a lower price is the result of cutting corners somewhere in the process. This can be dangerous for your health and safety, especially when it comes to something as vital as a surgical procedure.
Depending on the type of cosmetic procedure you’re seeking, some or all of the costs may be covered by insurance. However, it is important to remember that healthcare costs are continuing to rise and patients are increasingly responsible for higher deductibles, coinsurance and copayments.
It’s important to consider these increasing out of pocket expenses when evaluating your options for plastic surgery. It is also important to consider the benefits of nonsurgical alternatives, such as weight loss through diet and exercise. Cosmetic surgery is a serious commitment and should be reserved for only those who truly need it.
Associate Professor Dean White
The Avani Building, Suite 1, Level 1/12 Nelson Rd, Box Hill VIC 3128
(03) 9895 7631